Medicare Considers Coverage for Alzheimer’s Drug Aduhelm
- Written by Christian Simmons
Christian Simmons
Financial Writer
Christian Simmons is a writer for RetireGuide and a member of the Association for Financial Counseling & Planning Education (AFCPE®). He covers Medicare and important retirement topics. Christian is a former winner of a Florida Society of News Editors journalism contest and has written professionally since 2016.
Read More- Edited By
Lee Williams
Lee Williams
Senior Financial Editor
Lee Williams is a professional writer, editor and content strategist with 10 years of professional experience working for global and nationally recognized brands. He has contributed to Forbes, The Huffington Post, SUCCESS Magazine, AskMen.com, Electric Literature and The Wall Street Journal. His career also includes ghostwriting for Fortune 500 CEOs and published authors.
Read More- Published: August 30, 2021
- 3 min read time
- This page features 9 Cited Research Articles
- Edited By
The U.S. Centers for Medicare and Medicaid Services have begun a national coverage determination process to decide if Medicare will cover Aduhelm, a new Alzheimer’s drug. Aduhelm, also known as the medicine aducanumab, will receive a proposed decision on coverage within four months and a final decision in seven months, issued a CMS spokesperson to RetireGuide in a statement.
The Department of Veterans Affairs has already decided not to cover Aduhelm, according to The Wall Street Journal. The VA cited the potential for serious side effects and a lack of evidence that the drug is effective.
Since it was approved by the Food and Drug Administration (FDA) in June, Aduhelm has come under scrutiny over questions about the drug’s efficacy. According to The New York Times, multiple clinical trials in 2019 were shut down and failed to show significant evidence that the treatment helped people with Alzheimer’s.
Will Medicare Cover Aduhelm?
It’s too early to know if Aduhelm will receive Medicare coverage. The national coverage determination process, which began in June, takes up to nine months and includes several different stages, such as an initial decision and multiple public comment periods, to ensure a proper determination is made.
“We want to consider Medicare coverage of new treatments very carefully in light of the evidence available,” said Chiquita Brooks-LaSure, an administrator for CMS in an official company press release. “That’s why our process will include opportunities to hear from many stakeholders, including patient advocacy groups, medical experts, states, issuers, industry professionals, family members and caregivers of those living with this disease.”
But if CMS does determine that Medicare will cover Aduhelm, there are still complications. The drug, which is expected to cost $56,000 over a year, could financially hinder Medicare.
According to the Kaiser Family Foundation, Aduhlem could cost Medicare $29 billion a year if 500,000 beneficiaries get prescribed the drug.
Since Medicare typically only covers 80 percent of the cost of health care services, beneficiaries will have to pay a significant amount of money to receive Aduhelm treatment.
Even Medicare enrollees who do not need the drug could feel its impact. According to CNN, Medicare may have to offset the cost increase by raising premiums for its 60 million beneficiaries.
What Is Aduhelm?
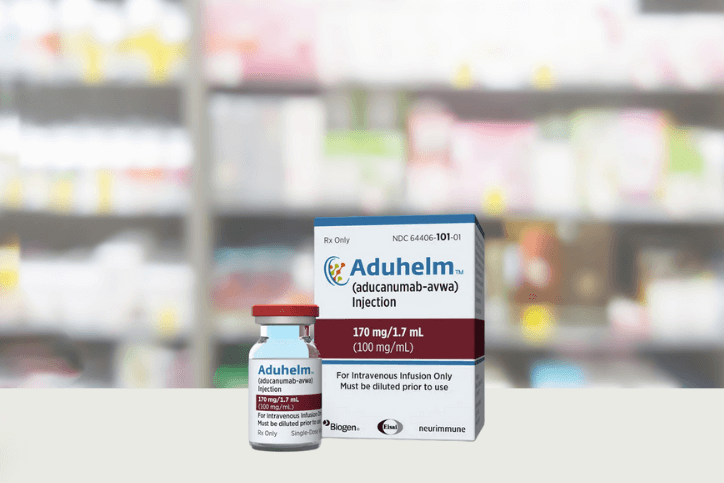
Biogen, a biotech company, developed Aduhelm to treat Alzheimer’s patients, but the drug has increasingly come under fire since its FDA approval.
The FDA commissioner has already asked for an independent review of the process that led to the drug’s approval, and two different congressional committees are also investigating that same approval and the drug’s price.
According to the Alzheimer’s Association, more than 6 million Americans have Alzheimer’s, and practically all those people are 65 or older. Aducanumab — marketed as Aduhelm — is the first drug that addresses the biology of the disease.
According to NPR, past Alzheimer’s treatments attempted to attack the amyloid plaques that form in the brain due to the disease. Aduhlem focuses on removing the amyloid entirely.
There is no cure for Alzheimer’s and effective treatments are limited.
Calling this number connects you to one of our trusted partners.
If you're interested in help navigating your options, a representative will provide you with a free, no-obligation consultation.
Our partners are committed to excellent customer service. They can match you with a qualified professional for your unique objectives.
We/Our Partners do not offer every plan available in your area. Any information provided is limited to those plans offered in your area. Please contact Medicare.gov or 1-800-MEDICARE to get information on all of your options.
866-749-5443Your web browser is no longer supported by Microsoft. Update your browser for more security, speed and compatibility.
If you need help pricing and building your medicare plan, call us at 844-572-0696